Faced with an explosion in the complexity of genomic, imaging and clinical data, AI is rapidly becoming an indispensable tool for oncologists.
In 2018, an artificial intelligence (AI)-based tool trained to identify skin cancer made headlines when it was found to miss fewer melanomas and misdiagnose fewer benign moles than 58 international dermatologists (Ann Oncol. 2018 Aug 1;29(8):1836-1842), leading to suggestions that machines might take over from clinicians.
Since then, AI has continued to gain momentum in oncology in the analysis of pathology samples and radiological images, with promising results for predicting prognosis and guiding treatment. However, prospective validation is still needed to ensure that successes from early studies can be repeated on a large scale and standardised, so that AI is implemented optimally across specialties such as oncology and pathology to improve patient care.
“Currently, we are at the point that we need to establish how AI-based techniques can be consistently implemented in hospitals that may have some variability in the way they prepare and stain samples,” explains Prof. Olivier Michielin, University Hospital of Lausanne, Switzerland. “I am absolutely convinced that AI will be responsible for an irreversible transition in oncology. It will be a fantastic tool for both clinicians and scientists – especially if medical experts drive the change and control the way AI is implemented.”
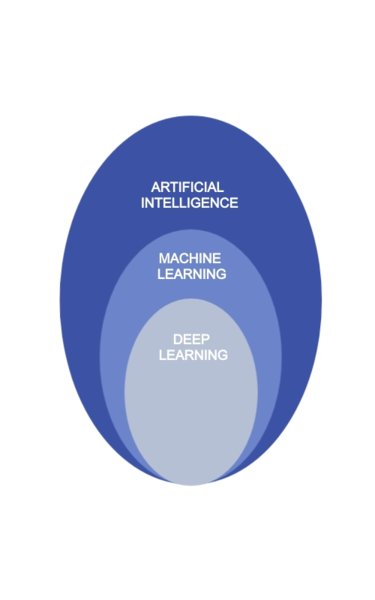
The term ‘artificial intelligence’ was first used in the 1950s (The History of Artificial Intelligence, 2006) and today it refers to a range of computational technologies that allow algorithms to mimic human intelligence (Cancer Science. 2020;111:1452–1460). These methods include machine learning which relies on statistical methods to detect hidden patterns within a dataset and improve performance with experience. Deep learning is a subfield of machine learning that harnesses the power of multi-layered networks.
Put simply, in pathology, AI uses algorithms to recognise similarities and differences between cells that the human eye cannot see. It can identify patterns in abnormal cells – down to the shape of nuclei – that the human brain cannot see. It can identify patterns in abnormal cells – down to the shape of nuclei – that the human brain cannot detect.
"Just as with AI-driven cars, we may not need our hands on the steering wheel all the time, but we need to be able to over-ride and take control when needed,” comments Prof. Viktor Koelzer, University of Zurich and University Hospital of Zurich, Switzerland. He explains that, if AI has to play a role in decision making, specific technical requirements will be needed to ensure that tools are reliable and robust (FDA, 2021; EU, 2021) particularly for features that are accessible only with advanced digital imaging and analysis methods.
Pathology and AI are natural partners in advancing cancer diagnostics but we need to define how they will work together.
“Regulators are discussing what these requirements should be and how performance can be standardised before these tools come to market, just like any other medical device,” he explains.
“In Europe, AI is taking a concrete form for the first time with the ‘Proposals for a Regulation laying down harmonised rules on artificial intelligence’ which has been recently released by the European Commission.”
AI algorithms in cancer diagnosis
Due to increasing interest and investment in the field, it is hard to keep pace with the rapidity at which AI systems are designed, developed and made available to healthcare professionals. In the USA and Europe, over 200 AI/machine learning-based medical devices were approved between 2015 and 2020, mainly in radiology and cardiology (The Lancet 2021; 3: E195-E203). In oncology, research reports have documented positive findings with AI models in the diagnosis of multiple cancers including lung, breast, thyroid and haematological cancers (Cancer Letters 2020; 471:61-71).
An FDA approved AI-based algorithm to aid prostate cancer diagnosis has recently been independently validated and shown to accurately detect, grade and evaluate clinically relevant findings in digitised slides of prostate core needle biopsies (Lancet Digital Health 2020; 2: e407–16). The tool identified a small number of cancers that had been missed during traditional analysis by pathologists.
“The algorithm showed high sensitivity and achieved almost perfect results for detecting true positive biopsies and ruling out false negatives in support of clinical experts,” says Koelzer. “It therefore has great potential to pre-screen samples and flag those for the pathologist to examine, and as a quality control tool to check for a positive result that may have been missed by the pathologist.”
Machine learning for delivering precision oncology
Machine learning models which adapt to new data when available offer the opportunity to guide decision making in the delivery of precision cancer care. Faced with an explosion in the complexity of genomics, precision oncology is the branch that can benefit the most from AI applications.
“If you train a machine learning system to understand which patients are doing well and which are doing poorly on a given treatment, it will start to make the link between the patterns it can detect and the likelihood of benefiting from that specific treatment,” explains Michielin. “With large amounts of high-quality data and images it should be possible for AI to pick up signals that can predict outcomes. One of the main limitations is the quality and relevance of the training data,” he adds.
Promising data have been reported with AI-based technologies for detection of molecular changes that can inform decisions about precision oncology treatment. In late-stage colorectal cancer, microsatellite instability (MSI) and mismatch-repair deficiency (dMMR) are predictive of response to immune checkpoint inhibitors, and deep learning has been shown to detect MSI and dMMR in tumour samples on routine histology slides faster and more cheaply than molecular assays (Gastroenterology 2020;159:1406–1416). In a large international validation cohort, a deep learning system detected colorectal tumour specimens with MSI with high sensitivity (Gastroenterology 2020;159:1406–1416).
A computer model trained to analyse high resolution images of histological slides has been shown to predict the molecular classification of colorectal cancer (Gut 2021; 70: 544-554). Tumours were classified into one of four distinct consensus molecular subtypes (CMS), based on the way cells and structures were organised, with potential for indicating optimal treatment strategies.
Koelzer, a member of the Stratification in Colorectal Cancer (S:CORT) consortium which performed the research, explains that this type of AI-based image analysis is still being validated and, if proven successful, may impact on the cost-effectiveness of molecular profiling. “If we can show that our algorithms achieve an equivalent level of performance to our current assays, we may be able to use these applications to screen patients more effectively in routine clinical workflows,” he adds. “In countries where molecular assays are unavailable, there may be added advantages in being able to upload images for diagnosis so that resources can be focused on the most appropriate treatment.”
Scalability is the big challenge
Standardising AI technology to generate the same resolution and quality of data wherever it is used will be key to future success. International initiatives such as the Standards for Reporting of Diagnostic Accuracy Studies (STARD-AI) Steering Group (Nature 2020; 26:807-808) are underway to standardise methodology and address questions of normalisation and acceptable levels of standard deviation.
In clinical testing, we need to train our AI systems as robustly as possible, so they are sensitive to patient characteristics and not to artefacts such as those arising from differences between study centres.
AI systems are currently trained on well characterised but limited cohorts, and an algorithm trained within a defined patient cohort may not perform as well on previously unseen cases.
“There is still a lot of work to translate our findings into the real world and validate them so they are widely generalisable. We also need to understand how our AI systems interpret the huge amount of data we generate, so we know how errors might occur,” adds Koelzer.
For example, in a recent study, human-computer collaboration for skin cancer diagnosis improved diagnostic accuracy over that of either AI or physicians alone, and the least experienced clinicians gained the most benefit (Nature Medicine 2020; 26: 1229-1234). However, it was found that faulty AI findings could mislead the entire spectrum of clinicians, including experts.
“If you are used to the AI system being right, it is very easy to believe what you are told, especially if you do not know how the system reached its opinion. Interpretability should be a key requirement for certification of these systems as they move into clinical practice so we can make the best decisions for our patients,” adds Koelzer.
Enhancing, not replacing oncologists
Michielin and Koelzer are quick to dismiss early suggestions that AI might replace oncologists or pathologists.
“AI will enable oncologists, pathologists and other stakeholders to work more efficiently, it will not replace them,” says Michielin.
Koelzer highlights the opportunities for improving the quality of patient care by automating many labour intensive, tedious jobs, especially now that clinicians are faced with such a huge increase in available data.
“In pathology, the vast majority of biopsy samples are negative, so if AI can rule out those samples, it will give specialists more time to use their human intelligence and all their experience and training to look at the remaining small proportion of results that are relevant, and make key decisions,” he says.
However, it will be important that specialists remain critical of the AI algorithms they use and not assume they have all the answers.
“Depending on the use of these tools, oncologists will need training to fully understand the boundaries within which AI can be used, so they do not trust predictions on questions that are beyond the training parameters which were used to build the algorithms,” says Michielin.
“The human brain is simply not capable of analysing and integrating the wealth of data we are now accumulating. We need AI to enable us to make the best sense of the growing complexity of our knowledge in cancer, and how to best use it for precision oncology,” he concludes.