Among the presented findings, a potential role for ESR1 gene fusions was observed
New insights into endocrine therapy resistance mechanisms in breast cancer were presented at the Molecular Analysis for Precision Oncology Congress (MAP) 2024 (London, 16–18 October), providing important information for guiding treatment.
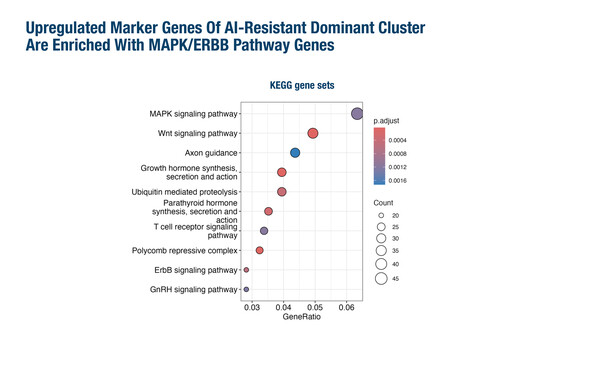
Most cases of oestrogen receptor (ER)-positive metastatic breast cancer ultimately develop resistance to endocrine therapy, which may be promoted by several factors, including mutations in the oestrogen receptor 1 (ESR1) gene in 20–40% of cases (Nat Rev Cancer. 2023;23:673–685). As presented in London, RNA sequencing analyses suggest that diverse mechanisms of resistance may arise contemporaneously in aromatase inhibitor (AI)-treated breast cancer (Abstract 108O). Single nucleus RNA sequencing revealed that AI-resistant ER-positive breast cancers were associated with features including ESR1 upregulation and decreased compositional heterogeneity, and were dominated by a cluster enriched in MAPK/ERBB pathway genes.
“The single nucleus RNA sequencing data showed distinct transcriptional subgroups of cells within the same cancer by gene expression clusters that have previously been associated with endocrine resistance,” observes Prof. Lajos Pusztai from the Yale Cancer Center, New Haven, CT, USA. He notes that although it is a small dataset, the findings support the growing evidence that many different drug resistance mechanisms may co-exist within the same tumour and lead to a phenotypic convergence. Taken together, these findings may explain why it has been so difficult to identify broadly applicable acquired drug-resistance markers and why re-treating patients after progression with a similar class of agent is often successful, because resistance is to a particular drug not to the pathway. Pusztai also notes: “It is important to bear in mind that rather than clonal selection, epigenetic transcriptional rewiring, which is partially reversible, is largely responsible for gene expression changes under therapeutic pressure (NPJ Breast Cancer. 2021;7:60).”
In a separate retrospective next-generation sequencing analysis, 38 gene fusions were identified in 35 (7%) of 503 breast cancers studied, and involved ESR1 in 53% of the observed fusion variants (Abstract 146P). The most frequent ESR1 fusion variant was ESR1-CCDC170 (78%), followed by ESR1-AKAP12 and ESR1-MTHFD1L. ESR1 fusions were linked to prior endocrine therapy use and were the sole drivers of potential endocrine resistance in most cases, with no simultaneous ESR1 mutations being observed.
“This study draws attention to another rare, but real, endocrine therapy resistance mechanism. However, in this study, the incidence of ESR1 fusion genes reported is much higher than that in previous reports, including those conducted by commercial molecular target profiling companies, which reported frequencies of around 1–2% (Ann Oncol. 2018;29:872–880; Cell Rep. 2018;24:1434–1444.e7),” comments Pusztai. He also cautions that not all fusion genes result in stable proteins. He concludes: “More detailed information on prior treatment histories, timing of biopsy, and associations between particular fusions and response to therapy are needed to judge the clinical utility of these findings. However, with the increasing adoption of RNA sequencing analysis as part of molecular target profiling, it is likely that fusion gene results will be part of future molecular diagnostics reports and could help predict response to therapies.”
Programme details
Patrikeev A, et al. Heterogeneity of endocrine resistance in estrogen-receptor positive breast cancer. MAP 2024, Abstract 108O
Proffered Paper Session 1, 16.10.2024, h. 13:30 – 15:00, Auditorium
Limaye S, et al. ESR1 fusions as potential mechanism of resistance to endocrine therapy in metastatic breast cancer. MAP 2024, Abstract 146P
Cocktail & Poster Display Session, 16.10.2024, h. 17:00 – 18:00, Foyer