In the OCLURANDOM trial, progression-free survival was longer in patients receiving lutetium-octreotate versus sunitinib
Encouraging data from the first multicentric randomised phase II trial of peptide receptor radionuclide therapy (PRRT) in patients with advanced pancreatic neuroendocrine tumours (NETs) were presented in a Proffered Paper Session at ESMO Congress 2022 (Abstract 887O).
[177Lu] Lu-DOTA-TATE (PRRT-Lu) was the first PRRT approved by the EMA (2017) and US FDA (2018) (EMA SPC; US Prescribing information) for the treatment of progressive somatostatin receptor positive gastroenteropancreatic neuroendocrine tumours (NETs) (Cancers (Basel). 2022;14:584). Although PPRT is rarely curative, it has been shown to help relieve symptoms, improve quality of life, shrink tumour lesions and slow disease progression (Cancers (Basel). 2022;14:584).
The OCLURANDOM trial was designed to evaluate the antitumour efficacy of PRRT with 177lutetium-octreotate (OCLU; octreotate is synonymous with DOTA-TATE) versus sunitinib in patients with somatostatin receptor scintigraphy (SSTR) positive unresectable progressive advanced pancreatic NETs. Previously treated patients with Eastern Cooperative Oncology Group Performance Status 0–2 and documented disease progression within 1 year prior to the start of the study were randomised 1:1 to receive OCLU (4 x 7.4 GBq infusions every 8 weeks) or sunitinib (37.5 mg/day) (NCT02230176). Forty patients were included in a single-stage Fleming design, with the conclusion that if 19 or more patients had no disease progression or death at 12 months, OCLU was considered effective. The sunitinib arm served as an internal control, with a 12-month PFS of 35% confirming the validity of the Fleming design hypothesis.
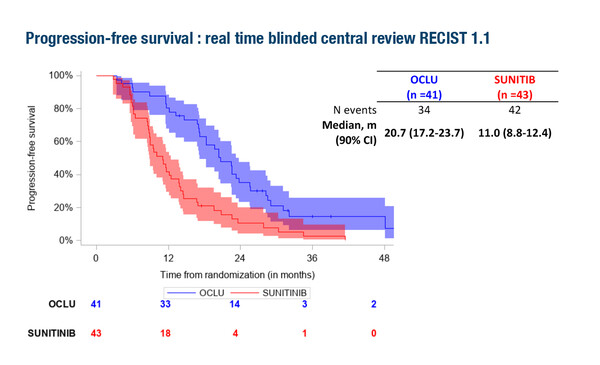
The study met its primary endpoint of achieving significantly longer progression-free survival (PFS) with PRRT with OCLU versus sunitinib within 12 months according to RECIST 1.1. Twelve-month PFS rates (RECIST 1.1 real-time central review) were 80.5% with OCLU (33/41 patients; 90% confidence interval [CI] 67.5–89.9) versus 42% with sunitinib (18/43 patients; 90% CI 29.1–55.5). Median PFS was 20.7 months (90% CI 17.2–23.7) in the OCLU arm versus 11.0 months (90% CI 8.8–12.4) in the sunitinib arm.
Patients in this trial had a mean age of 63 years and 52% were female. Of the 84 patients enrolled, 37% had Ki-67>10%, 42% had >25% liver involvement, 20% had functioning syndrome, and 43% had received two or more lines of systemic therapy. Grade 3–4 adverse events were experienced by 44% of patients in the OCLU arm versus 63% in the sunitinib arm, the most frequent including decreased blood cell count (12% versus 23%), digestive problems (12% versus 21%), hypertension (12% versus 19%) and fatigue (7% versus 12%). Drug withdrawal due to adverse events occurred in 5% of patients in the OCLU arm and 21% of patients in the sunitinib arm.
Dr Irene Burger, from Kantonsspital Baden, Switzerland, considered these data to be important, and advised that, “Despite the fact that the first clinical results for OCLU in SSTR-positive gastroenteropancreatic tumours were published back in 2003 (Eur J Nucl Med. 2003;30:417–422), randomised clinical trials investigating its impact on meaningful clinical outcomes were lacking. This is reflected in the 2020 ESMO Guidelines for gastroenteropancreatic neuroendocrine neoplasms and the European Neuroendocrine Tumor Society (ENETS) guidelines for neuroendocrine neoplasia, which state that due to a lack of randomised trial data, molecular targeted agents, such as everolimus or sunitinib, and systemic chemotherapy are the preferred treatment choices, and PRRT might only be considered after failure of these approved therapies (Ann Oncol. 2020;31:844–860; Neuroendocrinology. 2017;105:295–309; Cancers (Basel). 2022;14: 584). The current study therefore fills an important gap, despite some limitations such as the heterogeneity of prior therapeutic regimens.”
Abstract presented:
Baudin E, et al. First multicentric randomized phase II trial investigating the antitumor efficacy of peptide receptor radionucleide therapy with 177lutetium–octreotate (OCLU) in unresectable progressive neuroendocrine pancreatic tumor: results of the OCLURANDOM trial. ESMO Congress 2022, Abstract 887O
Proffered Paper Session, 12.09.2022, h. 16:30 – 18:00, Orléans Auditorium