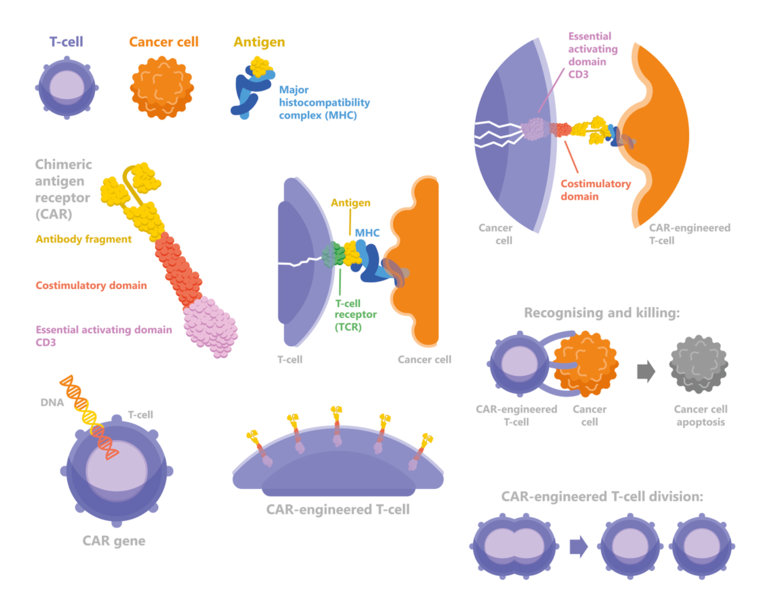
The benefits of adoptive T-cell therapy—where T-cells are given to induce a specific immune response—are moving closer to reality for patients with solid tumours
Studies presented at ESMO Congress 2019 over the past few days reflect the diversity of immunotherapies currently under investigation. At the beginning of what is likely to be a new era in cancer care, researchers have the technical expertise to use this approach for solid tumours, but it is yet to be determined which are the best targets and T-cell administration techniques.
Presented on Saturday, a phase I study in 9 patients with NY-ESO-1-expressing solid tumours who received T-cells genetically engineered to express a high affinity NY-ESO-1-specific T-cell receptor (TCR), reported persistence of modified T-cells. Three patients had detectable cells for more than 100 days post infusion and partial responses (n=2) were associated with significantly higher frequencies of CD45RA+ CCR7+ CD8+ T-cells (Abstract 1183PD). "These results support data from previous trials and confirm the validity of NY-ESO-1 as a therapeutic target,” says Dr Aurélien Marabelle from Gustave Roussy Cancer Center, Villejuif, France. "The most frequently used approach in this area is to transfer mixed populations of cells to patients. This study shows that efficacy appeared to be driven by a subset of T-cells with a clear phenotype and this perhaps highlights the importance of selecting the correct cells for treatment. We now need to know if there is any impact of the conditioning regimen—in this case cyclophosphamide—on response to treatment and this will be indicated by the durability of responses,” continues Marabelle. "With clear, durable responses, you can be confident that the T-cell therapy is likely to be active.”
On Saturday, antigen-specific T-cells induced by vaccination with blood-derived myeloid and plasmacytoid dendritic cells were reported to improve radiological progression-free survival (18.8 months versus 5.1 months in patients without antigen-specific T-cells, p=0.02) in a phase II trial in 21 patients with castration-resistant prostate cancer (Abstract 1179PD). Marabelle comments, "The finding that modified dendritic cells have an impact on survival is important. Improving ways of assessing efficacy, rather than just relying on survival outcomes—which requires large cohorts of patients and long follow-up times—may help to expedite investigation of new approaches.”
In this respect, advances in circulating tumour DNA technology—which were discussed at multiple sessions in Barcelona and covered in the Daily Reporter yesterday—may provide a solution to this, allowing oncologists to monitor treatment-associated changes in tumour kinetics and to adjust treatment accordingly. Findings from today’s poster session could help to overcome the limitation of the single-target specificity of T-cell therapies, which can lead to relapses in patients harbouring subclones of target-negative cancer cells. Marabelle also discusses the very preliminary findings of a study being presented today, which reports that HPV16 TCR-T and anti-PD-1-armoured HPV16 TCR-T-cells were safe and were associated with clinical activity in patients with advanced HPV16+HLA-A2+ cervical cancer (‘Poster Display Session 3’, 12.00 – 13.00, Poster Hall, Area 4; Abstract 1227P). "The important point about this trial in a virus-induced cancer is the co-expression in the same adoptive cells of an HPV-specific TCR and an anti-PD-1 short chain FV (scFV),” he says. "It is hoped that such genetically modified T-cells will be more efficacious as they will benefit from an intrinsic PD-1 blockade without the systemic adverse events of a regular anti-PD-1. On a separate note, targeting of a virus-specific epitope in this study is a good way to avoid antigens that are expressed in healthy tissues, which may help to explain the low toxicity of this treatment.”
According to Marabelle, while results look promising, major limitations of many of these early studies are the very small numbers of patients and short follow-up times. There are a variety of hurdles to be overcome before we see broad benefits from adoptive T-cell therapies for solid tumours in the clinic. These include issues related to T-cells ‘homing’ to the tumour—which might be overcome if T-cells are used ‘locally’; see Abstract 1226P—cancer cell recognition and destruction, and the heterogeneity of metastatic solid tumour cells. Cost is also a consideration but as with any innovation, initial high costs are driven down by competition and newer innovations, allowing the field to move forward. Despite the challenges, the oncology community is likely to see significant progress in this area in the next few years.
ESMO Congress 2019 abstracts:
- 1179PD - Natural dendritic cell vaccinations generate immune responses that correlate with clinical outcome in patients with chemo-naive castration-resistant prostate cancer
- 1183PD - Adoptive T cell therapy with TBI-1301 results in gene-engineered T cell persistence and anti-tumour responses in patients with NY-ESO-1 expressing solid tumours
- 1226P - A phase I clinical trial of malignant pleural mesothelioma treated with locally delivered autologous anti-FAP-targeted CAR T-cells
- 1227P - HPV16 E6-specific TCR-T armored with checkpoint blockade in the treatment of cervical cancer