Although bilobectomy remains a valid procedure, comparatively high mortality rates indicate that cautious use and appropriate patient counselling is required
Bilobectomy is a relatively uncommon procedure and perioperative survival outcomes are not well described compared with other pulmonary resections. In a Mini Oral Session at the European Lung Cancer Congress 2022, real-life data from a large US database show that perioperative survival after bilobectomy is worse than lobectomy and comparable to the outcomes of left pneumonectomy, highlighting the need for careful risk stratification and appropriate patient counselling before surgery (Abstract 109MO).
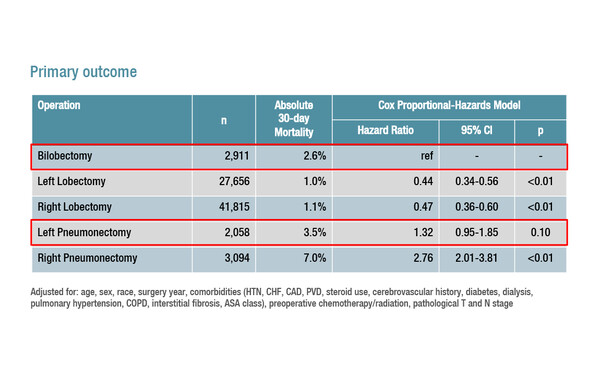
In this retrospective analysis of the Society for Thoracic Surgeons General Thoracic (STS) Surgery Database, patients were identified who underwent elective lobectomy (n=69,471), bilobectomy (n=2,911) or pneumonectomy (n=5,152) for lung cancer from 2009 to 2017. The primary outcome – 30-day perioperative mortality – occurred in 2.6% of patients who underwent bilobectomy, which was significantly more than in patients who had left lobectomy (1.0%; adjusted hazard ratio [HR] 0.44; 95% confidence interval [CI] 0.34–0.56; p<0.01) or right lobectomy (1.1%; HR 0.47; 95% CI 0.36–0.60; p<0.01). The 30-day perioperative mortality rate with bilobectomy was similar to that observed with left pneumonectomy (3.5%; HR 1.32; 95% CI 0.95–1.85; p=0.10), but better than with right pneumonectomy (7.0%; HR 2.76; 95% CI 2.01–3.81; p<0.01). Upper bilobectomy had a small but significant unadjusted 30-day survival advantage compared to lower bilobectomy (log-rank p=0.04).
It is striking that even when one lobe remains on the right side after bilobectomy, the mortality rate is comparable to when the whole left lung is removed.
“We therefore have to be very careful with our indications for bilobectomy, but I still think it is a valid procedure and, in terms of functionality, patients do benefit from having more lung parenchyma left behind,” says Prof. Isabelle Opitz from the University Hospital Zurich, Switzerland. “With all the revolutionary changes that are happening in thoracic surgery, such as the increasing use of minimally invasive surgery, it would be interesting to see if there were improvements in outcomes over the time period studied as one might expect to see lower morbidity and mortality rates in more recent years. Whether sleeve techniques were used in any of these interventions also warrants further analysis.”
Abstract discussed:
Li A, et al. Respect the middle lobe: perioperative survival of bilobectomy compared to lobectomy and pneumonectomy. European Lung Cancer Congress 2022, Abstract 109MO
Mini Oral Session 1, 31.03.2022, h. 17:00 – 18:00, South Hall 2