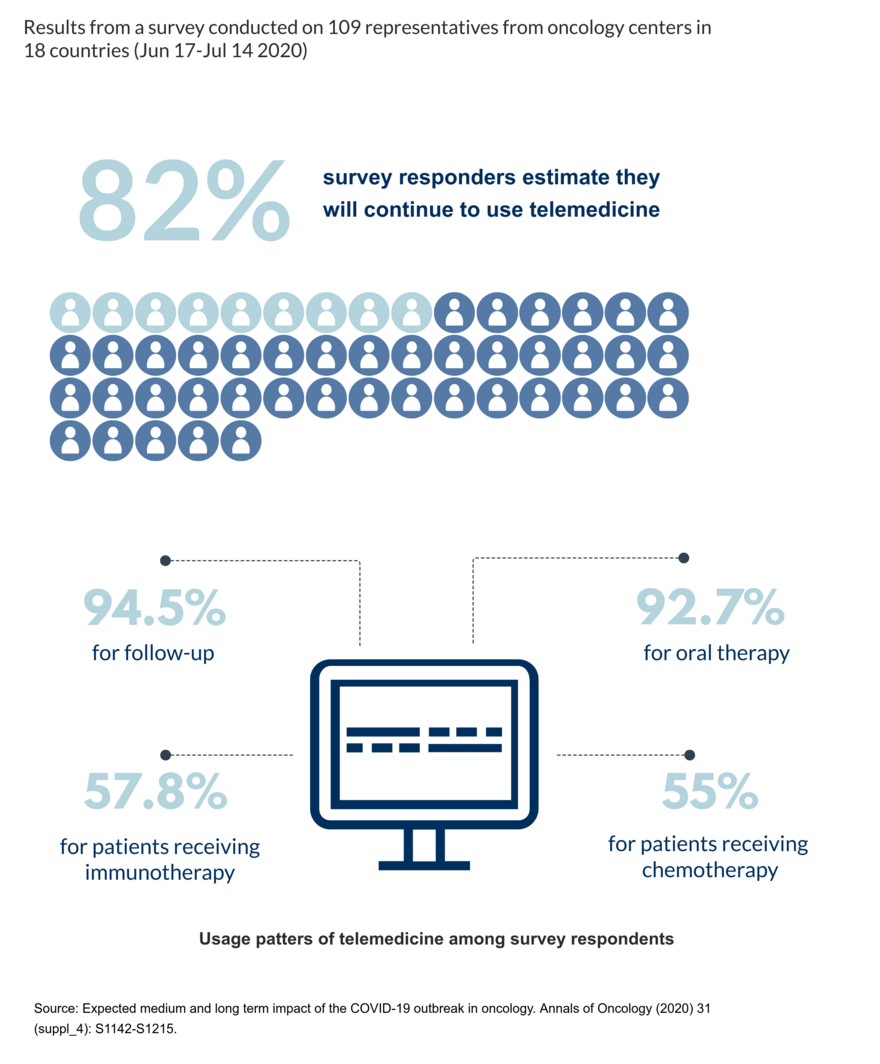
The start of a new pandemic era, with its imperatives to limit personal contacts and hospital visits, kicked off an unplanned race to digitalize oncology spurred on by necessity. In a global survey recently presented at the ESMO Virtual Congress 2020 aiming to assess the impact of the pandemic on the organisation of cancer care, which involved 109 representatives from oncology centers in 18 countries, participants reported to have made extensive use of teleconsultations for follow-up (94.5%), for oral therapy (92.7%), but also for patients receiving immunotherapy (57.8%) or chemotherapy (55%), and approximately 82% of participants estimate that they will continue to use telemedicine (LBA76_PR, ESMO Virtual Meeting 2020).. Whereas there is a legitimate need to find alternative solutions to assist patients remotely at any stage of cancer therapies, drawbacks of implementing digital services quickly exist as it is highlighted by the e-health expert Prof. Brian McKinstry from the Usher Institute at the University of Edinburgh, UK.
Telehealth, telemedicine, eHealth: what is the right term to use to describe this newly born process of digitalization in oncology?
These words have changed in definition over the last few years and are used quite loosely now. At the beginning, telemedicine referred just to video-consulting and then gradually became associated with other forms of clinical telemedicine, so involving both doctors and nurses. Telehealth was a broader concept which included non-clinical uses as well including, for example, virtual learning for healthcare professionals. Also, eHealth was used to define all digital tools in healthcare including also wearables or mobile apps. Many terms have emerged in the last years, some are very specific to medical specialties such as teleradiology or teledermatology, others are supposed to be omni comprehensive like telehealthcare. The truth is that it is a difficult territory as the terms are used differently by different people and definitions have changed over times.
Telemedicine is living a kind of a hype due to the pandemic. What are the potential benefits of improving telemedicine for patients and doctors?
There are two ways in which telemedicine has the potential to improve some aspects in medicine. One is that it is more convenient for patients not to have to go to a facility too often. People are likely to comply with medical appointments if they are conducted by telemedicine rather than face-to-face. Also, telemedicine can provide more frequent symptom and physiological data over a longer period than would normally be provided at a standard consultation. If you take blood pressure, for example, the classical way for people to manage hypertension is to see the patient 2-3 times a year to check blood pressure in clinics, while with telemedicine the patient's blood pressure can be checked remotely multiple times over the same period providing the doctor with a much broader range of results on which to make decisions. This ultimately results in reducing time for medical appointments for patients but also optimises resources in clinical settings. If implemented properly, telemedicine may reduce the workload for medical professionals.
What is the evidence that telemedicine fulfils its promises?
Despite the great hype generated around it in the last few months, researchers have worked for many years to produce evidence of its effectiveness in different settings. What we have seen so far is that telemedicine works well in some medical conditions, but it doesn’t in others. Overall, chronic diseases which require a continuum of care with frequent monitoring and active involvement of patients themselves offer the ideal settings for telemedicine services to be beneficial to both patients and doctors, but still some discrepancies are observed. Some projects have shown success in people with hypertension (PLoS Med. 2017 Sep 19;14(9):e1002389 - (BMJ. 2013 May 24;346:f3030), diabetes (J Telemed Telecare. 2019 Dec;25(10):587-601) and heart failure during the first months after being discharged from the hospital (Health Aff (Millwood). 2018 Dec;37(12):1983-1989). For other conditions like chronic obstructive pulmonary disease (COPD) and asthma, evidence is less secure. With my group I conducted several studies to investigate the impact of telemonitoring in COPD patients on detecting early exacerbations of the disease and reducing hospital admissions. Any well-conducted randomised controlled trial in COPD has failed to demonstrate any benefit to this population, but it has shown an unusual increased workload among healthcare staff (Am J Respir Crit Care Med. 2018 Sep 1;198(5):552-554.). Telemedicine may be acceptable as a model of care if it delivers service-level advantages such as reducing workloads or costs, but its role is still controversial.
What is the evidence for the use of telemedicine in oncology?
A very few studies have been conducted in oncology to evaluate the effectiveness of telemedicine services for different purposes. For instance, in a randomised controlled trial the combination of a telephonic care management and automated monitoring of pain and depression in cancer patients was conducted suggesting a potential benefit (JAMA. 2010 Jul 14; 304(2): 163–171), and in other studies telemedicine was associated with reduced costs (J Clin Oncol. 2009 27:15_suppl, e20508-e20508) and higher satisfaction and accessibility to cancer consultations like genetic counseling in patients living in remote areas (J Genet Couns. 2010 Oct;19(5):463-72). More recently, a pilot study showed the feasibility of using a remote video-assisted chemotherapy service to guide community-based nurses in delivering chemotherapy to cancer patients in rural areas who usually have more limited access to cancer services than people living in cities (J Clin Oncol.2018, no. 30_suppl (October 20, 2018) 82-82). Despite telemedicine promises to address several issues in cancer care, more research is needed, and the pandemic era may represent a major driver.
Are there any potential drawbacks from this current situation?
A few years ago, telemedicine was at the very top of the Gartner Hype Cycle, which every year provides a graphical visualisation of the lifecycle stages a technology goes through from conception to widespread adoption (see image). Although it has never entered the mature phase of integration into current healthcare systems, telemedicine is now living a second peak of inflated expectations in some medical settings where its potential was simply ignored for years. Teleconsulting, for example, which is the area that is really taking off in this pandemic, is a service that was hardly used up until a few months ago. In Scotland, we have been pushing and pushing it for the last three years with poor results in terms of a full integration into daily practice. I think that there were something like 2,000 teleconsultations in the last few years, while there have been 80,000 in the last six months alone.
“Although it has never entered into the mature phase of integration into current healthcare systems, telemedicine is now living a second peak of inflated expectations in some medical settings where its potential was simply ignored for years.”
I think that for certain types of consultations like psychological and psychiatric problems video consulting is superior to phone consulting. But with the work we did in this area, we also discovered that video consultations tend to be short and to be focused on one problem whereas face-to-face consultations often deal with multiple problems.
What are the potential consequences of having implemented telemedicine service so quickly?
I think that there is a real risk of unmet expectations in the future. Things done too quickly could be done badly, with risk of increasing the workload rather than reducing it and this may lead some medical professionals to think that telemedicine is not a good option while if it was well-planned they might see it differently. One thing that is important to highlight when it comes to telemedicine is that technology is not “the solution”, rather it is only a catalyst for a change of how cancer care is delivered and medical staff is organised. So, it is very important that whenever a new system is introduced in a workplace, staff get adequate training and time to get to terms with it, and that they see concrete benefits of its effectiveness in daily practice. People are always a key factor to a successful use of a technology.
Are patients another important driver to the successful implementation of a new digital service?
Absolutely. Patients generally like telemonitoring, in every piece of research that we have done it has been popular. Problems may depend on the level you want to run the new system at, if it requires patients to have some form of internet connection and/or a smartphone which they must be able to use. In this case, the new telemedicine service will exclude some people like the very poor, those with cognitive difficulties and some elderly. We must to be very cautious about what service we want to offer to our patients and make sure that the systems that we introduce are very simple to use and also accessible to everyone. Some systems work on simple text which can work also on very old-fashioned mobile phones, they have the advantage of being easy to use, and also to be universally held. However, the newer systems in smartphones can do much more, can integrate better into electronic medical records, and as the time goes by more and more people have these devices. What we have to remember also is that not everybody uses the features of these smartphones, they may have a smartphone but they do not do anything other than phone calls, texts occasionally or take photographs, but they do not use apps.
Is patient empowerment critical to the implementation of telemedicine?
It is quite complicated to explain to patients the concept of risk associated with therapies and how treatment works, so oncology is a difficult area. On a general rule, the more the patients are informed about their condition, the more likely they are to adhere to treatments. So, I think it does make sense to use whatever system we have to try to improve the knowledge that patients have about their condition.
Is the involvement of telemedicine experts in the design of new services beneficial to their success?
I think it is because one of the major problems is that for many clinicians it is difficult to judge what software or digital device works and what does not, particularly when they have very little time to make an informed decision. This makes healthcare professionals in general more vulnerable to aggressive marketing strategies from leading companies who try to get people to buy complex systems without prior assessing how they could be implemented in a real scenario. My biggest advice is to find colleagues who are already using these systems because whenever you speak to companies who are selling their products, all you get is hype. So, getting in touch with doctors and nurses who have already gone through this change in daily routine is by far the best thing to do to understand successes and pitfalls of telemedicine.