The updated Antineoplastic Medicine Survey (ANMS) dataset shows that essential therapies remain out of reach for patients in most low and lower middle-income countries despite international efforts
The recently published “ESMO Global Consortium Study on the availability, out-of-pocket costs, and accessibility of cancer medicines: 2023 update” (Ann Oncol. 2024;Article in Press), the largest study of its kind, gathered data by 317 reporters and 231 peer reviewers from 126 countries. The results urged its co-first author Prof. Nathan Cherny, Shaare Zedek Medical Center, Jerusalem, Israel to call on policymakers, non-governmental organisations (NGOs) and medical oncologists worldwide to leverage the results for more effective action to ensure equitable access to high-quality cancer treatment.
Prof. Cherny, two previous ESMO studies on the availability, out-of-pocket costs and accessibility of antineoplastic medicines in Europe (Ann Oncol. 2016;27(8):1423-1443) and outside of Europe (Ann Oncol. 2017;28(11):2633-2647) had comprehensively mapped the vast disparities in access to cancer treatment that exist between high-income and low and middle-income countries. Why repeat this research, and what does the new data teach us?
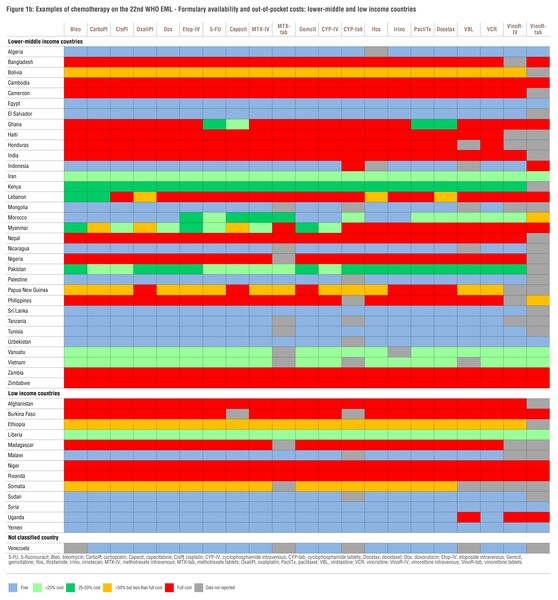
The survey was repeated in 2023 to obtain updated data and understand what happened in the five years since the original survey: a period during which various initiatives were launched by ESMO, the World Health Organization (WHO), and other actors to improve access to essential, high-value medicines which are the foundation of high-quality cancer care. Unfortunately, the results show a largely unchanged landscape. According to updated data, patients in high-income countries have generally access to treatment, including to the more expensive new medicines with high clinical benefit on the ESMO-Magnitude of Clinical Benefit Scale, at little or no out-of-pocket cost. Meanwhile, in low and lower middle-income countries, access even to basic generic anticancer medicines and old chemotherapies on the WHO’s Model List of Essential Medicines (World Health Organisation 2021:pp67) remains limited and associated with significant financial toxicity for patients and their families.
To put it plainly, this means that cancer patients in most of the developing world either do not get any treatment for their disease at all, or receive medications that are no longer the standard of care. Where newer, targeted agents would be indicated, these are usually unaffordable or inaccessible because the required molecular testing is either not available or not reimbursed, as described by another global ESMO study on this subject (Ann Oncol. 2023;34(10):934-945).
How do you explain the slow pace of change on this issue, and what can be learned from the countries that did see progress in recent years?
Access to medicines can be affected by various factors such as which therapies are included on a country’s drug formulary, how much they cost, and what proportion of that cost patients themselves have to assume. Upper middle-income countries such as Argentina, Brazil, China, Kazakhstan and Türkiye have succeeded in improving access to chemotherapy, hormonal agents, and even to some of the more expensive new medicines through better reimbursement and coverage. One factor contributing to this progress is that various countries have recently improved their health technology assessment (HTA) structures.
However, the issue remains complex with aspects including healthcare system organisation, governance, and economics which can be difficult to solve in low-income settings. Even in countries with strong healthcare planning such as India, resource limitations mean that patients have to pay out of pocket for cancer medicines including the most basic. Realistically, the barriers to access in certain regions will not be overcome in the short term without extensive philanthropic support.
What impact do you hope this study will make?
As a global community, we want all cancer patients to be able to benefit from the medical and scientific developments of the last 20 years. Thanks to the collaboration of hundreds of contributing reporters, our study is providing a unique snapshot of inequities in access to cancer care across 126 countries and shows that efforts made thus far have not been sufficient. The value of such a dataset is that it can be used to support global actions, for example by the WHO for its global monitoring and other activities in low and lower middle-income countries, as well as by individual countries to identify gaps in the accessibility and affordability of vital anticancer medicines. Importantly, it can also serve to inform the work of a number of NGOs that have become increasingly involved in attempting to improve access to essential cancer medicines through philanthropy in recent years.
Being a medical oncologist myself, individually and as a profession we should recognise our own role as stewards and advocates for high-quality cancer care in our local communities and worldwide. Accessibility is key irrespective of your country’s income level: we, medical oncologists can have a relevant voice in international initiatives to improve access to care globally.
What part do you believe ESMO can play in addressing the challenges identified?
As a reference for oncology education and information with a global perspective, ESMO will continue to monitor the situation on a regular basis as part of the Society’s core commitment to making high-value cancer medicines accessible and affordable to all patients who need them.