Author: Dr Dario Trapani, European Institute of Oncology (IEO), Milan, Italy
The health of a population is based on effective health services, which rely on truthworthy data for correct health planning process. In oncology, the development of National Cancer Control Plans (NCCP) is instrumental to outline programmes for cancer care, thus informing resource allocation and defining responsibilities and leadership roles, while ensuring accountability and monitoring of health impacts. According to the World Health Organization (WHO), NCCP is a ‘public health programme designed to reduce the number of cancer cases and deaths and improve the quality of life of cancer patients. The development and design of NCCP must be shaped from a country situational analysis and aim to portray the status of cancer burden based on cancer incidence and mortality data.
The health planning process has the ultimate role to serve every person and seek to improve the wellbeing of people. Therefore, the foundation for tailored policies to address the specific health and social needs of patients deserves high quality data, particularly specific metrics on cancer burden.
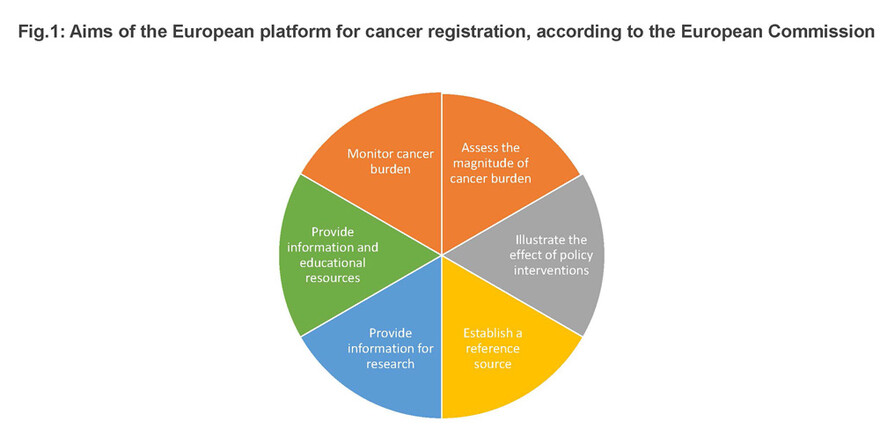
The European (EU) Cancer Information System (ECIS) is a web-based platform that encompasses data from 150 EU population-based cancer registries. ECIS was developed under the auspices of the EU Directorate-General for Health and Food Safety, as an initiative of the European Commission's Joint Research Centre, to foster the Regional collaboration and co-operation of cancer registries affiliated to the European Network of Cancer Registries. The aim of ECIS is to provide updated quantitative health metrics on the EU cancer burden and develop projections to explore regional variabilities and temporal patterns.
A key strength of ECIS is its ability to monitor health-related progress in response to the implementation of policies, including the uptake of innovative cancer treatments, for example new medicines in oncology. Ultimately, a high-quality cancer registry is crucial for implementing evidence-based systematic and equitable interventions for the prevention, early detection, diagnosis, treatment and palliation of cancer. Ensuring consistency in data management and that all relevant stakeholders have transparent access to, and are able to share data, are critical features to guarantee the comparability of estimates across countries with the aim of providing equitable cancer-related governance.
The health of a population is based on effective health services, which rely on truthworthy data for correct health planning process.
Recently, the European Commission’s Joint Research Centre and WHO’s International Agency for Research on Cancer (IARC) have estimated the cancer burden in European countries for the year 2020, utilising the ECIS framework. Updated results will be presented during the ESMO 2020 Virtual Congress (Abstract 1581O).
Projections for 2020 among European Union Member States reveal a rise to 2.7 million in absolute new cases of cancer, and 1.3 million deaths. An age pattern was reported, with up to two-thirds and three-quarters of the respective new cases and deaths affecting persons aged 65 years or older. Sex disaggregated data showed that more than 1.2 million new cases were in women and more than 1.4 million cases were distributed in men.
The most common cancer types were breast, colorectal and lung in women and prostate, lung and colorectal in men. The estimates for breast cancer confirmed its leading incidence across all age groups: in women aged up to 44 years, breast cancer accounted for 38% of all new diagnoses. In men, prostate cancer accounted for 23% of all cancer diagnoses. However, for the younger adult male population, nearly one-third of diagnoses in the 20–39 years age range was ascribed to testicular tumours.
The leading causes of mortality in EU countries were breast, lung and colorectal cancers in women and lung, colorectal and prostate cancers in men. Interestingly, lung cancer was the leading cause of death in adult women aged 45–64 years and in all men older than 45 years, accounting for up to one-third of all the mortality burden. Cervical cancer is still a major cause of cancer mortality among young women (10% of cancer deaths in women under 45 years of age).
Notably, some of the figures are subject to geographical variability related to disparities in the implementation of evidence-based effective cancer interventions across the cancer continuum. Updated results from this joint effort reporting from EU Member States only will be presented at ESMO Virtual Congress 2020 (Abstract 1581O).
The capacity of governments to deliver high-impact quality cancer care is based on the ability to formulate data-informed health policies. Hence, a detailed situational analysis at a national, regional and global level is a key step in implementing effective cancer policies that are sensitive to gender differences and the pursuit of equity in all healthcare in priority areas for cancer control. Without quality data, there would be no quality cancer care to all.
Session details
- Dyba TA et al. Estimation of European cancer burden for the year 2020. ESMO 2020, Abstract 1581O
- Proffered Paper - Public Policy, 21.09.2020, h. 14:25 - 16:05, Channel 2