Retrospective data suggest that patients with low baseline TILs and nodal involvement have poor prognosis despite achieving pathological complete response
As presented at ESMO Breast Cancer 2025 (Munich, 14–17 May), a retrospective study found that low baseline stromal tumour infiltrating lymphocytes (TILs) and nodal involvement could predict a subset of patients who remained at risk of relapse despite otherwise appearing to have a favourable long-term prognosis (Abstract 2O).
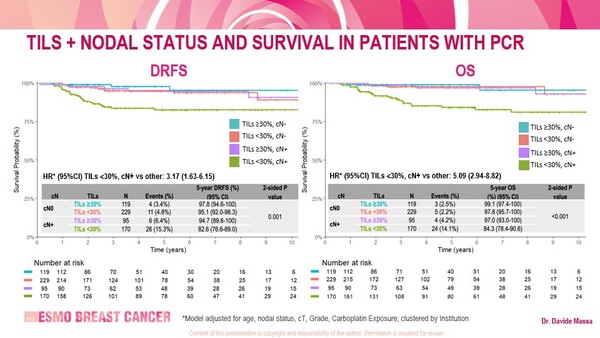
The study involved 613 evaluable patients with stage I–III triple-negative breast cancer (TNBC) who achieved a pathological complete response (pCR) following neoadjuvant chemotherapy (NAT). With a median follow-up of 4.2 years, low baseline TILs (<30%) and nodal involvement were independently associated with worse outcomes than high TILs (≥30%) and no nodal involvement. At 5 years, distant relapse-free survival (DRFS) and overall survival (OS) were 82.6% and 84.3%, respectively, for patients with baseline TILs <30% and nodal involvement compared with 97.8% and 99.1%, respectively, for those with TILs ≥30% and no nodal involvement (p=0.001 for DRFS and p<0.001 for OS). Patients received chemotherapy (anthracyclines [95.3%], taxanes [86.5%], carboplatin [49.6%]) and/or immunotherapy (20.4%) prior to surgery. Findings were confirmed in sensitivity analyses that excluded patients treated with immune checkpoint inhibitors.
An association between high baseline TILs and improved outcomes has been widely reported in patients with early-stage TNBC, both in the adjuvant (J Clin Oncol. 2019;37:559–569) and neoadjuvant settings (Clin Cancer Res. 2024;30:2160–2169), and also in the absence of chemotherapy before/after surgery (JAMA. 2024;331:1135–1144). “However, the role of TILs for risk stratification in patients who achieve pCR has previously been underexplored,” says Dr Kevin Kalinsky from the Emory Winship Cancer Institute, Atlanta, GA, USA. “Results from the retrospective study are intriguing and may help to further refine our thinking in terms of patients who might be at risk after receiving NAT, despite achieving a pCR.” He acknowledges that the findings are hypothesis generating and that further ongoing studies may confirm this effect. He adds: “Now the question is, would giving these patients additional treatment after surgery improve their outcomes?”
Programme details
Massa D, et al. Integrating tumor infiltrating lymphocytes and nodal status for risk stratification in patients (pts) with triple-negative breast cancer (TNBC) and pathological complete response (pCR) after neoadjuvant treatment (NAT). ESMO Breast Cancer 2025, Abstract 2O
Proffered Paper Session 2, 15.05.2025, h. 14:00 – 15:30, Room 14