Two studies provide new insights on the effects of vaginal oestrogen therapy and physical exercise to tackle sexual impairment
Issues impacting sexual health are common in women following a diagnosis of breast cancer, with genitourinary syndrome of menopause (GSM) and negative body image as common drivers. Despite the widespread use of topical hormonal treatments to relieve the symptoms of GSM, there continues to be a level of uncertainty about their safety in hormone-sensitive cancers, including breast cancers, particularly in patients receiving aromatase inhibitors.
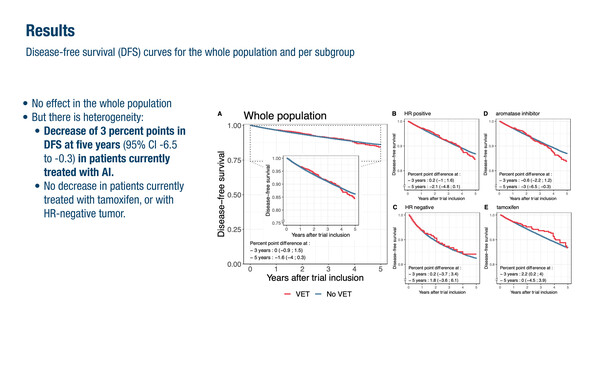
At ESMO Breast Cancer 2024 (Berlin, 15–17 May), a population-based target trial emulation indicated that while vaginal oestrogen therapy (VET) appeared to be safe for individuals with hormone receptor (HR)-negative tumours and those receiving tamoxifen, there were some concerns in HR-positive patients treated with aromatase inhibitors (Abstract 268MO). Using nationwide data from French insurance claims, the study investigated the potential impact of VET in 1,739 women out of a total cohort of over 134,000. VET use was associated with a detrimental effect on 5-year disease-free survival (DFS). “A decreased DFS of 2.1% and 3.0% were reported in HR-positive patients and in those concurrently receiving aromatase inhibitors, respectively,” says Dr Don S. Dizon from the Lifespan Cancer Institute, Providence, and Rhode Island Hospital, Providence, USA. A greater reduction in DFS was observed following oestriol than promestriene (−4.2% versus 1.0%, respectively, at 3 years). “These results are in line with data from a Danish national cohort study (J Natl Cancer Inst. 2022;114:1347–1354). However, neither reports on the impact on mortality from breast cancer (if any) or other causes. In addition, caution is needed because of different effects based on the type of VET used and also the dose, the duration and the frequency of use. Despite these data, the totality of the evidence supports the use of VET for sexual health issues, but it does require a careful and balanced conversation with all women, weighing up the benefits and the potential risks,” he notes.
Non-pharmacological interventions such as physical exercise represent a valuable option to offset a decline in physical wellbeing and health-related quality of life in women during and after the end of cancer therapies (Breast Cancer. 2022;29:402–418), but their impact on sexual impairment is difficult to gauge. Also presented in Berlin, a randomised study reported that a 9-month supervised exercise programme was associated with a sustained improvement in sexual functioning (p=0.0031) and endocrine sexual symptoms (p=0.0026) at 6 months compared with usual care (Abstract 269MO). The PREFERABLE-EFFECT trial involved 355 women with metastatic breast cancer from five European countries and Australia, with almost half of sexually active women reporting little or no sexual enjoyment. Around one in four reported moderate-to-severe endocrine sexual symptoms and a similar proportion reported a negative body image. The exercise programme consisted of providing general exercise advice to participants who received an activity tracker.
“These findings broadly describe what is known about sexual function and desire,” remarks Dizon. “If someone is not feeling well – they may be experiencing fatigue and nausea, for example, from their treatments – they are unlikely to have much sexual interest. By improving fatigue, exercise can improve quality of life, and this can have a knock-on effect on sexual health. And it is good to see that this is true, even in the metastatic breast cancer setting,” he says.
According to Dizon, more needs to be done to improve the management of sexual health in breast cancer survivors by raising greater awareness among medical oncologists. “We in the medical community need to embrace the concept that sexual health is frequently impacted after cancer and, as such, it should part of the general health review for all our patients,” he concludes.
Abstracts discussed:
Dumas E, et al. Safety of vaginal estrogen therapy after early-stage breast cancer: a nationwide population-based target trial emulation. ESMO Breast Cancer 2024, Abstract 268MO
Mini Oral Session 2, 17.05.2024, h. 08:30 – 10:05, Hamburg Hall
Schmidt ME, et al. The effects of exercise on sexual health and breast cancer-specific symptom burden in women with metastatic breast cancer: Results of the multinational randomized PREFERABLE-EFFECT trial. ESMO Breast Cancer 2024, Abstract 269MO
Mini Oral Session 2, 17.05.2024, h. 08:30 – 10:05, Hamburg Hall