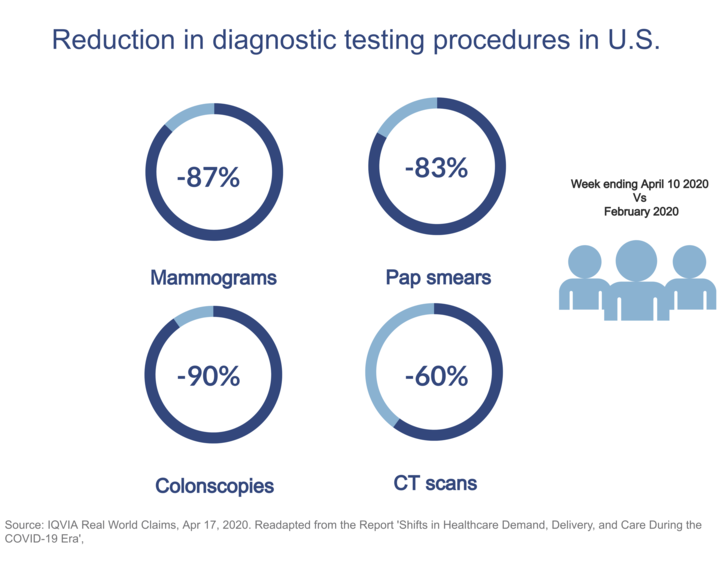
A few months on from a partial shutdown of what were considered non-urgent healthcare services – including cancer screening programmes – some drops and delays in cancer diagnoses have already been documented (Lancet Oncol 2020 June; 21:750-751). Now that several countries are once again tightening preventive measures in the face of rising COVID-19 case numbers, another potential reorganisation of healthcare is not far off and some are raising the alarm about indirect effects of the pandemic on global cancer mortality and morbidity.
“Only 10 percent of screening programmes have been able to continue in the past few months”, says Dr Richard Sullivan, King’s College London, UK, who co-led the development of the COVID-19 and Cancer Global Taskforce, among other things, to assess the impact of the pandemic on cancer outcomes. “Initial results of the Taskforce survey on global cancer screening show that about half of screening programmes have been only partially open and as many as 40 percent of the world’s screening activities are still suffering a complete shutdown.”
According to Sullivan, the disruptive effects of this will increase inequalities between countries. “While high-income countries with organised national screening programmes have the capacity to reopen relatively quickly during the pandemic, in low and middle-income countries restarting screening activities within small regional or charity programmes is going to be incredibly difficult,” he says. “In many of these places it will take anywhere between 12 and 24 months to restart.”
Dr Ophira Ginsburg, Director of the Perlmutter Cancer Centre High Risk Programme at NYU Langone Health in New York, USA, Co-chair of the Prevention working group within the COVID-19 and Cancer Global Modelling Consortium (CCGMC), a part of the Taskforce, shares this concern: “Nine out of 10 women who die of cervical cancer live in low and middle-income countries, because they do not have access to effective screening and treatment programmes – it is the epitome of cancer health disparities and this pandemic is sure to make things worse,” she highlights.
“Having people missing or waiting several months for a screening is a real cause for concern”
Bringing people back to hospitals
Social distancing measures, which are part of daily routine in healthcare since the COVID-19 outbreak, are another aspect that make screening units operate at lower capacity as Ginsburg reports from her own experience. The patients she sees carry mutations that give them an individual breast cancer risk of up to 60 percent for BRCA 1 and 2 genes or, in the case of Lynch syndrome, particularly predispose them to early-onset bowel or uterine cancers. “Our patients are proactive individuals: they have been diligent about maintaining their appointments and we have been fortunate to be able to absorb the backlog,” she says, sharing her concerns for other high-risk subjects who have not been screened yet. “About one in 300 Americans has a Lynch gene and one in 200 women in the US carries a BRCA genetic mutation, but the vast majority are not aware of it. In individuals with Lynch syndrome, for instance, the time sequence in which a benign polyp becomes an invasive cancer is greatly accelerated. That is why the fact that some of them missed or waited several months for a screening through standard prevention pathways is a real cause for concern.”
Even where screening services have been able to reopen, however, there has not been a return to normal care. “The problem is also bringing patients back, because it seems that people are not turning up as they should,” says Sullivan. “Have they just forgotten or are they still frightened to visit hospitals? In the UK, for example, there is still an incredible amount of bio-fear. Social science research is needed to understand these behavioural patterns towards screening in pandemics.” Based on the behavioural changes observed in past crises, however, Sullivan is pessimistic: “People simply stop going to their screenings because of financial instability or fatalistic attitudes that set in. This is a really insidious effect that hits the lowest socio-economic groups the hardest.”
Toward this direction, Ginsburg and her colleagues in the Prevention working group of the CCGMC are currently assessing how people’s risk behaviour has changed during the pandemic, focusing also on socio-economic aspects that may be drivers. “So many people have already lost their jobs and it is easy to imagine that this is going to lead to an increase in behaviours that are commonly associated to cancer risks,” she says.
“We are already seeing people come in with advanced cancer who should have been diagnosed in February.”
Dark statistics are expected also for common cancers
How many people are missing their opportunity for early cancer diagnosis as a result? Some warn that disruptions in diagnostic services seem to be associated with a delayed presentation of asymptomatic patients missing the screening path as well as symptomatic patients, not timely referred to the appropriate care path. Sullivan has seen a worrying trend emerge in the UK: “Screening programmes have reopened to significant backlogs, but the diagnostic backlog for examinations like endoscopies and colonoscopies is much worse: currently 12 to 18 months and growing,” he reports. “We are already seeing people come in with advanced cancer, who had symptoms and should have been diagnosed in February.”
According to recent predictive modelling, 3,500 additional deaths at five years from diagnosis can be expected in England due to current delays in diagnostic processes across breast, lung, oesophageal and colorectal cancer (Lancet Oncol. 2020; 2020 Aug;21(8):1023-1034). Underlining that this estimate covers the impact for only four major tumour types in England and from diagnostic delays alone, Sullivan adds that it concerns relatively young individuals who might have had a chance of being cured if their disease had been detected earlier. “COVID-19 compressed the mortality we would have had anticipated over the next year. The additional cancer deaths we can expect due to delays in healthcare provision, meanwhile, are going to weight with a significant proportion of years of life lost in addition to the deaths for COVID-19,” says Sullivan.
Making predictions is still challenging
In these very days when the perspective of new – at least partial – lockdowns is not unrealistic in some countries, many efforts are put into analysing indirect consequences of policies on cancer care. At the global level, the total impact on cancer mortality and morbidity threatens to be even more far-reaching. The Global Modelling Consortium aims to extract what screening delays are going to really mean in terms of downstream mortality and years of lost life, although high uncertainty makes modelling a hard exercise. “I believe, however, that most of the fallout will be due less to the virus than to the way health policies are implemented and received,” comments Sullivan.
Ginsburg, who volunteered on the wards during the period when her programme was shut down, recalls a time when it sounded reasonable to take certain decisions in clinical care. “At my institution, there was not a unit dedicated to COVID-19 patients and the whole hospital was potentially a place where you could get sick,” she says. “New York quickly became the global epicentre for infections and, sadly, for deaths. Back then, adopting very strict measures was a consequence of what we knew at the time. But we learned so much having gone through it that I do not think we would ever shut some essential health services like cancer screening programmes again.”
Sullivan concludes that the oncology community should learn from the recent past and try to act differently to deal with an exacerbating emergency. “The oncology community, like other disease communities, needs to make treasure of the first wave of the pandemic and reflect honestly on some mistakes that were made. We shut services down based on false epidemiological modelling that predominated in the early days of the outbreak. Decision-makers and the clinical community have learnt how the abrogation of health service is critical, resulting in direct and indirect impacts on healthcare - which is going to hit worse the younger population.”