Recent findings show digital tools have the potential to improve the monitoring of symptoms and psychological aspects, but they should be integrated within routine clinical practice
Digital therapeutics may help to prioritise patient wellbeing in cancer care, as suggested by an expanding body of research (J Med Internet Res. 2025;27:e69621; Health Technol. 2025;15:243–272; Ann Oncol. 2024;35(Suppl 2):S1172).
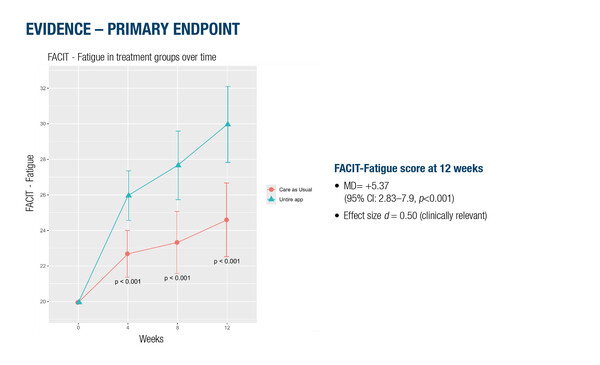
Several presentations at the ESMO Congress 2025 (Berlin, 17–21 October) focused on the impact on patient quality of life (QoL) and other outcomes of a number of digital approaches currently in development. Data on the effectiveness and safety of a multimodal digital therapeutic (the ‘Untire’ app) to help patients self-manage cancer-related fatigue (CRF) were presented from a multicentre, randomised controlled trial of 200 breast cancer survivors with moderate-to-severe CRF receiving maintenance therapy (Abstract 2545MO, key results in the box below). At 12 weeks, the app significantly reduced CRF (FACIT-Fatigue), fatigue severity (Brief Fatigue Inventory) and QoL (FACT-G), and improved global functioning (Clinical Global Impressions scale) and distress (Distress Thermometer) compared with usual care.
A further multicentre, randomised trial reported a lower rate of clinically meaningful QoL deterioration over 24 months of follow-up among 404 evaluable survivors of head and neck cancer (HNC) (post curative treatment) who used a mobile app with a coaching chatbot (BD4QoL platform) compared with those who received standard clinical follow-up (LBA49, key results in the box below).
“Digital tools enable patients to track outcomes and symptoms with their clinicians, in addition to enabling access to advice on the management of symptoms and side-effects in real time, making access to care much faster,” says Dr Madeline Pe from the European Organisation for Research and Treatment of Cancer in Brussels, Belgium. “We are now in an era where most people have access to a smartphone, so there has been a cultural shift over recent years where individuals have become less sceptical of using digital tools and mobile applications as a way to manage their health.”
The need to develop novel approaches in supportive care is urgent in order to address psychological aspects, which still represent an issue for many patients. Findings presented at the ESMO Congress, in fact, revealed decreased emotional functioning (EF) scores, indicative of some degree of depression and/or anxiety during cancer diagnosis or treatment, in a real-world study of 1,450 patients with solid tumours receiving systemic therapy (Abstract 2544MO, key results in the box below). Median EF scores of 66.7 on a scale of 0–100 were reported across the study cohort, with lower scores indicating worse emotional state. Women, younger patients (<62.5 years) and those receiving palliative care tended to report worse emotional functioning compared with men, older patients and those undergoing curative treatment.
“We normally assess depressive symptoms and other psychological issues using standardised and validated questionnaires and these are often done when a patient visits their relevant healthcare professional,” says Pe. “With the use of digital tools to monitor patients’ symptoms and wellbeing, we hope to capture more real-time feedback on how patients are feeling, enabling psychological support to be provided earlier.”
“But an important caveat is that these tools should never replace the healthcare professional: they are there to provide additional support. The clinician and patient should discuss and review the use of these tools together to ensure that they address the needs and preferences of the patient.”
Integrating digital technologies into the patient journey presents some challenges. For instance, not all digital tools are the same, with each tool providing a different type of support strategy to address the needs of a specific patient population. In addition, evidence of the benefits of these tools are based on outcomes that are often measured over the short term, so it will be important to determine whether benefits are maintained over time and if patients engage with their use over a longer period. Other challenges relate to uptake by clinicians and building and maintaining a digital infrastructure within a hospital environment, including optimal integration within the clinical workflow.
A further consideration is the impact of digital tools on healthcare costs, which are often perceived as a major barrier to their integration in routine workflows. Health economic modelling has shown potentially reassuring results: an average benefit of approximately €260 per patient per month was associated with integration of an active e-health support compared with an information-only approach, as reported in a study of patients with breast cancer (Abstract 584P, key results in the box below). “The cost savings are usually attributed to earlier interventions preventing serious adverse events, which translates to a reduction in hospitalisations and emergency care. As with any health economic modelling, the presented findings are based on specific assumptions, in this case, those relevant to the German healthcare system. Understanding these assumptions is important to support informed decision-making,” advises Pe.
Given the QoL benefits demonstrated with digital approaches in many studies, these findings suggest that a shift toward the integration of digitally assisted, patient-centred support tools as part of routine cancer care is increasingly likely. “This has been an active area of research for decades; we have learned how to build on the work of several groups to develop interventions in such a way that they fit with clinical workflows and address the needs of both patients and clinicians. It takes time to translate research into clinical practice, but hospitals are starting to be more open to investing resources in digital infrastructures and I think there will shortly be an increased uptake of these tools. It will also be interesting to see how artificial intelligence transforms this field in the near future,” concludes Pe.
At a glance:
Starzer AM, et al. Monitoring the development of depressive symptoms in real-world patients with solid cancer under systemic therapy. ESMO Congress 2025 - Abstract 2544MO
- Women vs men: median (m)EF scores 61.1 vs 66.7; p<0.001
- Younger (<62.5 y) vs older patients: mEF scores 66.7 vs 75.0; p<0.001
- Palliative vs curative setting: mEF scores 66.7 vs 75.0; p=0.001
- Highest mEF (75.0 in older male colorectal cancer patients
- Lowest mEF (41.7) in younger female patients with other cancers
Spahrkäs S, et al. Effectiveness and safety of a multimodal digital therapeutic for cancer-related fatigue in breast cancer survivors: A multicenter randomized controlled trial. ESMO Congress 2025 - Abstract 2545MO
- Significant reduction in week-12 fatigue using Untire app vs usual care (primary endpoint: MD FACIT-Fatigue = +5.37; 95% CI 2.38–7.9; p<0.001; d=0.50), clinically relevant
- Significant improvements with Untire app for BFI and QoL, and consistent improvements in tertiary outcomes (CGI scores [clinician- and patient-rated], HADS and distress)
- >80% of pts engaged regularly
Cavalieri S, et al. Primary endpoint analysis of the BD4QOL study, a multicenter randomized trial for monitoring quality of life by intelligent tools in head and neck cancer survivors after curative treatment. ESMO Congress 2025 - LBA49
- At 24 months, pts with 10-point decrease in EORTC C30 GHS for BD4QoL platform vs control: 10.2% vs 20.1%; p=0.006
- At median 18.1 months of follow-up, median GHS deterioration-free survival not reached in both arms: HR (unadjusted Cox model) = 0.46; 95% CI 0.27–0.78; p=0.0041
Harbeck N, et al. Integrating e-health support in advanced breast cancer care: Impact on healthcare costs and patient outcomes. ESMO Congress 2025 - Abstract 584P
- AeHS generated average benefit of ~€260/patient/month under German healthcare system assumptions
- Estimated monthly AeHS value for base-case scenario using WTP of €200,000/QALY and €21,000/SAE
- Primary driver of financial benefits: reduction in hospitalisation and emergency care costs