OnCOVID study reveals that respiratory symptoms, fatigue and cognitive/psychological dysfunction persist after acute Sars-CoV-2 infection, with an impact on survival and oncological outcomes after recovery
Sequelae from infection with SARS-CoV-2 (COVID-19) have recently emerged as a major unknown of the pandemic era, now that more evidence has been collected on the impact of the acute COVID-19 syndrome and the effectiveness of COVID-19 vaccination in patients with cancer. According to the OnCOVID study, the results of which will be presented on 21 September at the ESMO Congress 2021 (Abstract 1560O), sequelae post-COVID-19 compromise long-term survival and outcomes, affecting up to 15% of patients with cancer after recovery (based on a total of 1,557 patients with cancer who survived COVID-19).
Persistent ill health after acute COVID-19 – referred to as long COVID, the post-acute COVID-19 syndrome, or the post-COVID-19 condition – is a matter of concern for all healthcare providers, including medical oncologists as there are many unanswered questions on the long-term impact on prognosis and cancer care following COVID-19.
In the study, conducted in the UK by Imperial College London from 27 February 2020 to 14 February 2021, researchers reported that at a median post-COVID-19 follow-up of 128 days, sequelae were associated with a 76.0% increase in the risk of death (hazard ratio [HR] 1.76; 95% CI 1.16–2.66), after adjustment for sex, age, comorbidities, tumour characteristics, anticancer therapy and COVID-19 severity.
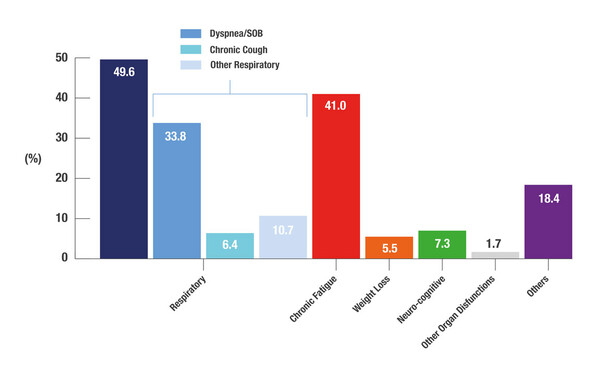
Sequelae included respiratory symptoms (49.6%), fatigue (41.0%) and neuro-cognitive issues (7.3%), with persisting effects significantly more common in males, patients aged ≥65 years, those with at least two comorbidities, and those with a history of smoking (Figure 1). Patients with previous hospitalisation for COVID-19, prior complicated COVID-19 or who had received COVID-19 therapy were also significantly more likely to have post-COVID-19 sequelae.
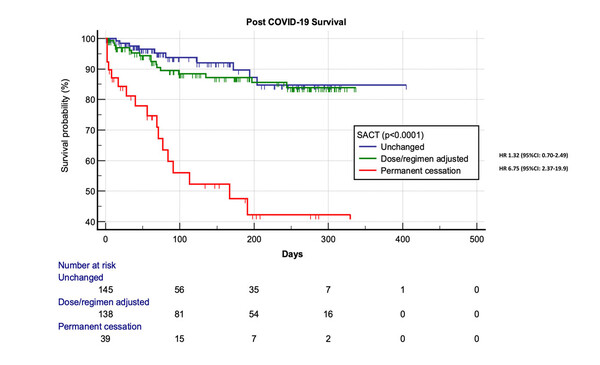
In terms of cancer management, 14.8% of 471 patients receiving systemic anticancer therapy (SACT) at the time of COVID-19 diagnosis required permanent discontinuation of treatment. This was associated with a 3.5-fold increased risk of death (HR 3.53; 95% CI 1.45–8.59).
The main reason for therapy discontinuation was worsening performance status (61.3% of patients). There was, however, no adverse impact on survival of SACT dose/regimen adjustments (Figure 2), which were reported in 37.8% of patients. Adjustments were made mainly to avoid hospital attendance (25.8%), immunosuppression (50.0%) or adverse events (19.1%).
The scheduled completion of the OnCOVID study is expected in 2022 when more information regarding the impact of COVID-19 on the treatment and outcomes of patients with cancer will be available.
Cortellini A et al. Prevalence and impact of COVID-19 sequelae on treatment pathways and survival of cancer patients who recovered from SARS-COV-2 infection. ESMO Congress 2021, Abstract 1560O
Proffered Paper session – SARS-CoV-2 and cancer – 21.09.2021, h. 14:10 – 14:20, Channel 5