Findings from international registries improve knowledge on how to manage cancer care in the pandemic era
Results from three international registries presented at the ESMO Congress 2021 today prove that older age, comorbidities, active cancer, more advanced cancer and immunosuppressive chemotherapy are all associated with a higher risk of suffering a severe COVID-19 infection, as early studies in the pandemic era previously suggested.
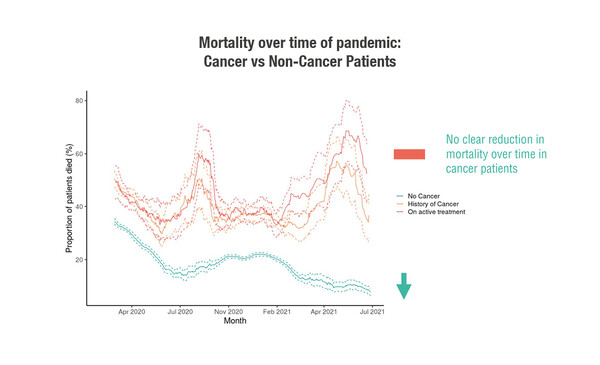
Cancer is an independent risk factor for death from COVID-19, data from the Clinical Characterisation Protocol (CCP)-CANCER-UK confirm. This is Europe’s largest prospective hospitalised COVID-19 dataset, involving more than 20,000 patients with cancer. Among hospitalised patients with cancer and COVID-19, younger patients (<50 years) on active cancer treatment were 5-times more likely to die than similar-age non-cancer patients (adjusted hazard ratio 5.22; p<0.001) (LBA60). With data up to August 2021, there was no downward trend in mortality among cancer patients over the course of the pandemic. Another study, from a Swiss national registry, reported that cancer patients had a mortality rate more than 12-times that of the general population, with rates of 21.5% among 455 cancer patients and 1.7% in the general population (Abstract 1570P).
However, findings presented today also suggest that there was a time-dependent improvement in COVID-19-related mortality rate over the course of the pandemic (Abstract 1565MO). Data for 2,634 cancer patients from the European OnCovid registry suggested that 14-day case-fatality rates fell from February–March 2020 to January–February 2021 (29.8% versus 14.5%, respectively; p<0.0001). The difference likely reflects improvements in testing and healthcare resources, and temporal changes in community transmission of COVID-19.
Dr Luís Castelo-Branco, Medical Oncologist at the ESMO Scientific and Medical Division and a member of the steering committee for the international ESMO-CoCare Registry, which presents its first report at the ESMO Congress 2021 (Abstract 1567MO), suggests that the enormous amount of information collected by these registries on cancer patients with COVID-19 will prove invaluable in terms of lessons learned. Results from the ESMO-CoCare Registry includes information from 20 countries for more than 1,600 patients with any solid or haematological malignancy who had a COVID-19 diagnosis, and revealed that the majority (64%) of participants in this database had severe COVID-19 necessitating hospitalisation, with 31% subsequently dying and 11% requiring intensive care. Conversely, 97% of patients with non-severe COVID-19 recovered, with stage I–II cancer associated with greater likelihood of recovery than stage IV cancer at COVID-19 diagnosis (odds ratio [OR] 3.11; p<0.001). Severe COVID-19 was associated with poor ECOG performance status (OR 3.18 for a score of ≥2 versus 0–1), haematological malignancies (OR 0.51 for solid versus haematological cancers), and active/progressive cancer status (OR 1.89 versus no evidence of disease). While male gender, older age, non-Caucasian ethnicity, low body mass index and presence of comorbidities were also linked to severe COVID-19, caution is warranted in the interpretation of the results owing to potential selection bias.
Although these studies were reporting data up to as late as August 2021, in the case of the CCP-CANCER-UK study, much of the information would have been collected prior to the wide availability and uptake of COVID-19 vaccines. The picture may be considerably different now for cancer patients who have been fully vaccinated, and research assessing the impact of the vaccines specifically in these more vulnerable populations will add an important dimension to knowledge about the severity and consequences of COVID-19 infection in cancer patients.
How would findings from these registries inform current clinical practice? “As healthcare professionals, we should appreciate that this is very much a dynamic situation. As vaccination rates increase, the world will move from a global pandemic towards better control in some regions but poor control in others,” Castelo-Branco responds. “We should use the best evidence available to select the most suitable treatment options for patients, including those with COVID-19 infection, and keep discussing with patients their COVID-19 vaccination plans. Secondly, keep investing and co-operating in the research process; there are still so many unknowns, including the long-term effects from COVID-19 and long-term vaccine effectiveness in patients with cancer, on which some early evidence has been presented at the Congress. Finally, given that burnout rates in health professionals have soared during the pandemic, it is now more important than ever to take care of ourselves and our colleagues.”
Maintaining and reinforcing global collaboration is key to helping all those around the world who might be facing situations of endemic COVID-19 in the months and years ahead, according to Castelo-Branco. “The outstanding co-operation between different groups around the world has been essential to increasing our knowledge on the effects of COVID-19 in the cancer population,” he says. “We should recognise that we have access to all this information – collected in what is a very short time-frame – only because researchers, oncologists and patients agreed to contribute and share their data. We now need to work through it and understand the clinical findings so that we can apply them moving forward from the pandemic.” Reflecting on the challenges faced in setting up ESMO-CoCARE and other global initiatives and sharing ideas for overcoming obstacles will be an important part of ensuring the more rapid and reliable collection of information across countries.
Palmieri C et al. Prospective data of >20,000 hospitalised patients with Cancer and COVID-19 derived from the International Severe Acute Respiratory and emerging Infections Consortium WHO Coronavirus Clinical Characterisation Consortium: CCP-CANCER UK. ESMO Congress 2021, LBA60
Mini oral session – SARS-CoV-2 and cancer, 21.9.2021, h. 16:45 – 16:50, Channel 2
Pinato D et al. Time-dependent improvement in the clinical outcomes from COVID-19 in cancer patients: an updated analysis of the OnCovid registry. ESMO Congress 2021, Abstract 1565MO
Mini oral session – SARS-CoV-2 and cancer, 21.9.2021, h. 16:50 – 16:55, Channel 2
Romano E et al. COVID-19 and cancer: first report of the ESMO international, registry-based, cohort study (ESMO CoCARE). ESMO Congress 2021, Abstract 1567MO
Mini oral session – SARS-CoV-2 and cancer, 21.9.2021, h. 17:00 – 17:05, Channel 2
Joerger M et al. Outcome and prognostic factors of COVID-19 infection in cancer patients: Final results of SAKK 80/20. ESMO Congress 2021, Abstract 1570P